Based on the original article “Using a Brain-Based Foundation for Preparing and Supporting Families,” featured in NACAC’s quarterly newsletter, Adoptalk
I have worked in the world of foster care and adoption since 2004.
One of the most heart-breaking parts of my work has been seeing everyone trying, I mean really trying, and feeling like a failure.
It happens with all members of the community: kids, parents, professionals. I am guessing you can relate.
My world turned upside down—or maybe right-side-up—when I learned that children (and the adults who care about them) are acting exactly as their brains have been wired to act, and, even more importantly, that we can change our brains!
Suddenly, the shame lifts, and we can deal with the real stuff: the brains, bodies, and relationships. I have spent the last decade diving deep into developmental neuroscience, helped in large part by my colleague, Dr. Jonathan Baylin (co-author of Brain-Based Parenting and The Neurobiology of Attachment-Focused Therapy). My mission now is to bring the research to life in practical ways for brave kids and all the adults in their lives.
Attachment and the Brain: Getting to the Real Issue
We now know just how vital a healthy attachment system is for brain development. Since all behavior comes from the brain, it is essential that we address this root issue—in children and caregivers. I often begin trainings with some simple truths:
- Trauma is not being sure I have the resources to survive. Infants are a little bundle of needs, completely dependent on others to meet those needs. It is no wonder those early difficult experiences can have such a lasting traumatic impact.
- Trauma sets my nervous system up for a life of survival on my own.
- Trying to survive on my own can lead to some behavior that others don’t like (and that might not serve me well in the long run).
- Healing relational trauma happens in relationship. Remember, superheroes are born from adversity. No one needs our pity, but they might need our presence.
This should be integrated into every part of our work.
We want to send signals of safety to parents in prevention programs. After making the difficult decision to remove a child from a dangerous setting, we should be making every effort to earn the trust of parents and family members so we might be a resource and coach toward reconnection with their child.
We should foster relational health in the workplace, reducing the push to do more than humanly possible as social workers and advocates.
We should infuse our training and support of foster and adoptive parents with a deep understanding of what is happening in the brain and how that impacts behavior. Keep reading for practical information to share with families.
The Brain’s Two Operating Systems: An Explanation for Parents and Kids
The brain has two main operating systems: social-approach/engagement mode or “upstairs brain” and defense mode or “downstairs brain” (Siegel and Bryson, 2011). At birth, the downstairs brain is the operating system at work. This system is home to primal feelings like terror and rage. The infant cries out, and the loving parent rocks and soothes and tries to meet the child’s need. It takes thousands of repetitions of this call-and-response to start building neural highways to the more advanced operating system—the upstairs brain.
We use our upstairs brain to:
- Connect with others
- Problem-solve and deal with complexity
- Control impulses and strong emotions
- Develop empathy
- Tolerate frustration and boredom
- Play and enjoy interactions
- Learn, analyze, and change
Even with great care and connection, we humans all have times when the downstairs brain takes over.
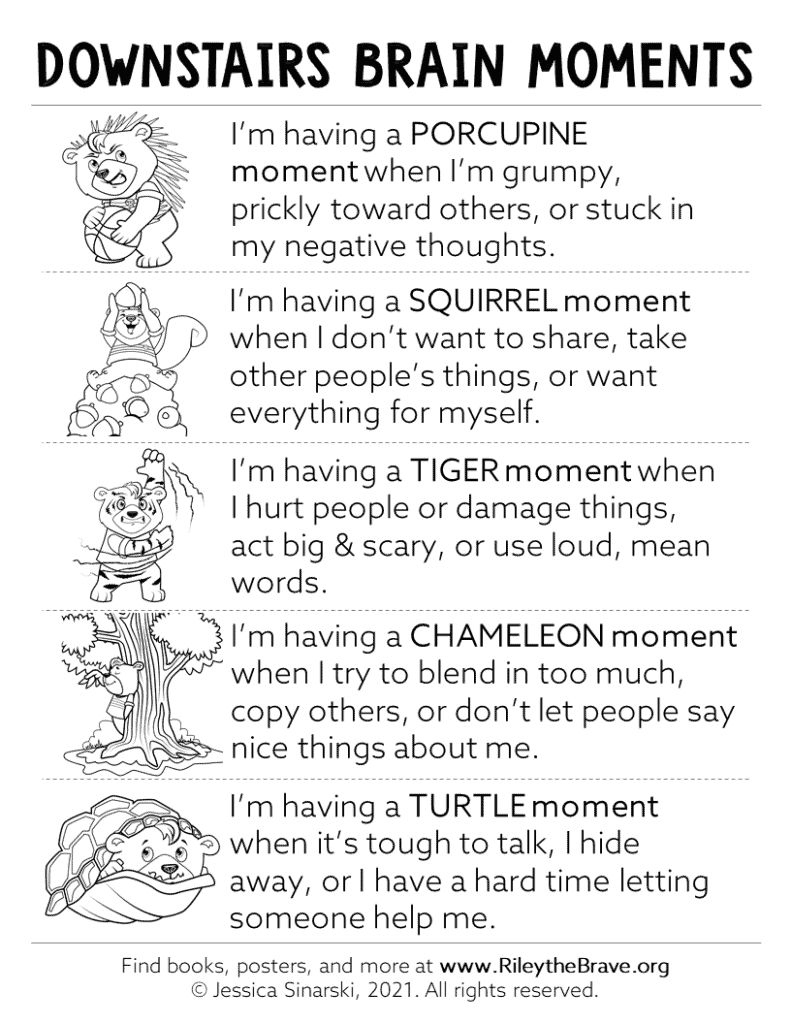
I gently introduce five different “downstairs brain moments” in the picture book, Riley the Brave (2020). Remember, the same things that kept kids alive can get them in trouble later. It is essential that we recognize the courage of survival—times when children have had to keep others away by being prickly or hiding away like a turtle, instead of simply seeing these downstairs brain moments as bad behavior.
When an infant or young child experiences trauma, especially the loss of a birth parent, they adapt to their dangerous life by strengthening, and primarily using, their downstairs brain. Unfortunately, that operating system does not seek—or at times even recognize—safety, logic, or connection.
Unsurprisingly, youth can get stuck in a cycle of solo survival characterized by the big feelings and challenging behaviors that often leave parents at their wits’ end and seeking professional help.
Mental Health Disorder vs Adaptive Behavior
Parents frequently come into my office having received terrible advice, harmful and inaccurate diagnoses, and excessive medications from mental health professionals.
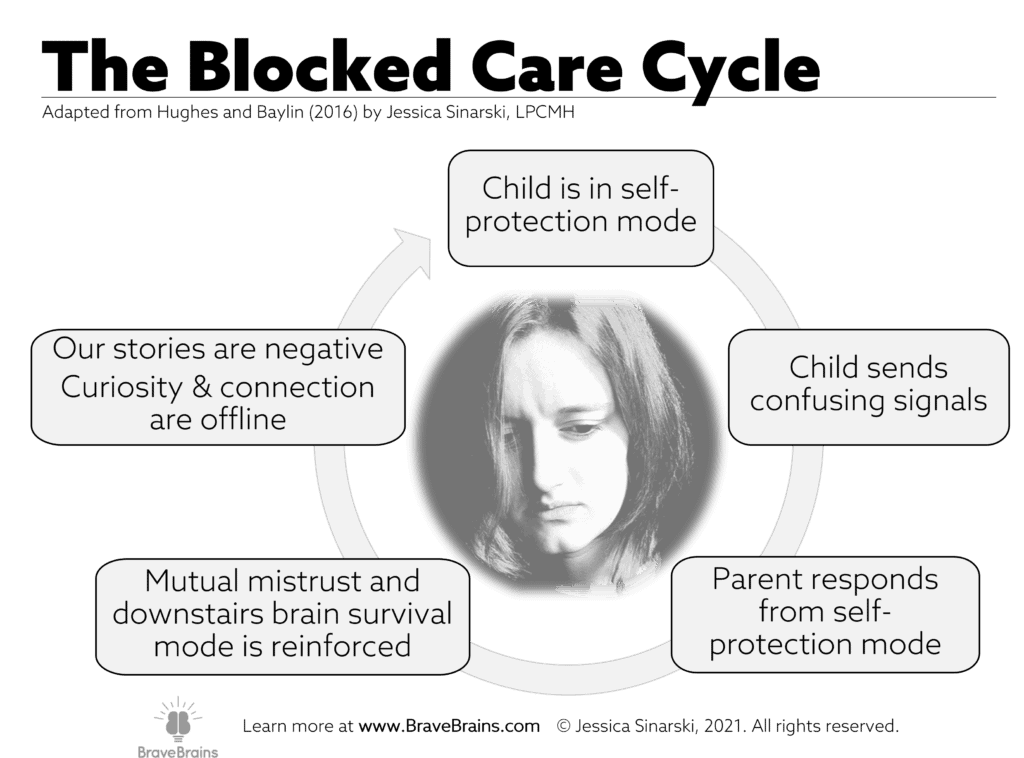
So many of the kids (and parents) in the world of foster care and adoption have adapted to systemic oppression, toxic stress, and poor care by shutting down the parts of their nervous system that seek connection, that “upstairs brain” operating system. Instead, they have needed to be ready for solo survival. What emerges is blocked trust (Hughes and Baylin, 2016).
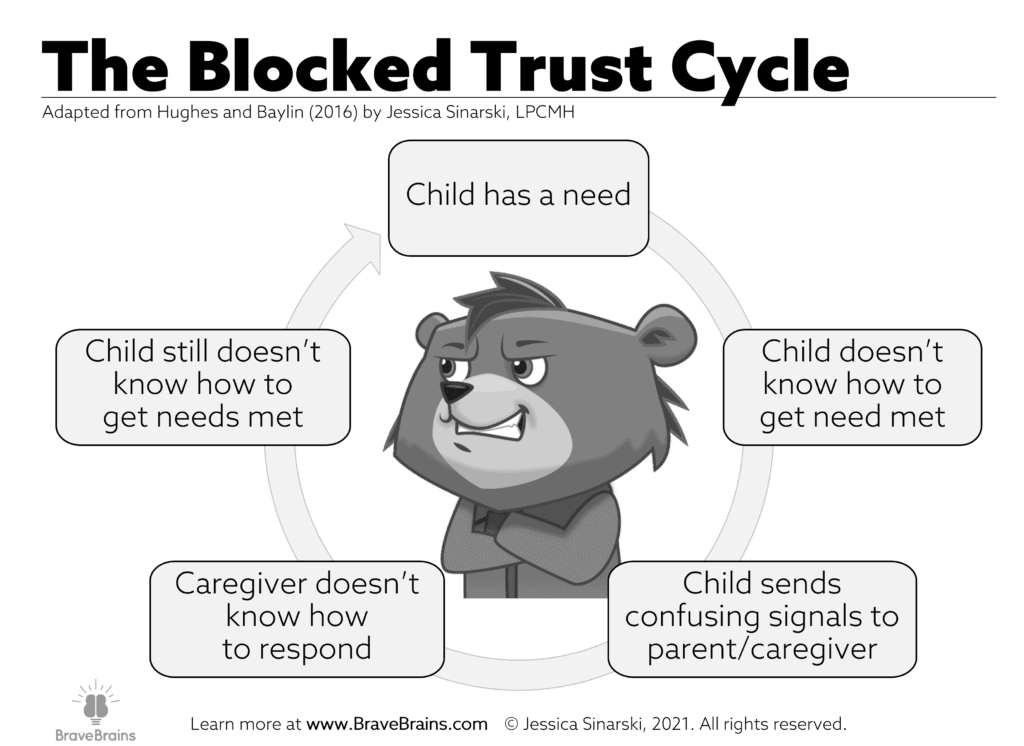
While there are certainly times that underlying mental health issues might be present and medication can be helpful, we do families a disservice if we do not first explore the attachment issues in play. Those “confusing signals” in the blocked trust cycle are often the very behaviors that dominate conversation in school and counseling settings.
If you are thinking, “Confusing signals? What does that look like in real life?“
Think about defiance and disrespect. These are frustrating behaviors, but with our brain-based lens we can see the child might really be saying, “I haven’t learned if I can trust anyone to be on my side.”
Likewise, stealing often means, “I have learned to provide for myself, and it’s hard to depend on you instead.” Talking with a child about their “squirrel moments” can be a playful way of helping them recognize the need they are trying to meet instead of staying stuck in the cycle of defense and mistrust.
When parents, social workers, and teachers begin to interpret these “downstairs brain moments” as misplaced brave moments, we can help brains built for mistrust and self-protection find more calm, curiosity, and—importantly—safe connection.
It’s incredibly powerful, but it isn’t easy, especially for parents who are on the receiving end of lots of tiger and porcupine and turtle moments with their kids and teens.
Preventing and Treating Blocked Care
Parenting is difficult in the best of circumstances.
The rage, defiance, and rejection that accompany a child’s blocked trust make parenting even harder. Many of the feel-good brain chemicals, like oxytocin and dopamine, are in short supply for kinship, foster, and adoptive parents. While children’s brains control their behavior, it is natural for parent brains to be affected by the behavior more than what is going on inside the child’s brain. It becomes terribly painful to keep trying, to keep caring.
Remember, our brains are protective! So, parent brains start to distance from the child or teen that is sending out self-protective prickly porcupine spikes. Without support, blocked trust naturally leads to blocked care, which typically looks like defensiveness, apathy, or a complete loss of hope.
Warning signs of blocked care (Corkum and Qualls, 2020):
- Loss of curiosity and compassion for the meaning behind a child or teen’s behaviors.
- Feeling defensive and irritable or ashamed
- Feeling burned out, overwhelmed, and fatigued
- Isolating from other parents
- Feeling cynical about helpful ideas
- Loss of all pleasure in parenting
Keep in mind, professionals, you are not immune to blocked care as you work with parents.
Because we often naturally have compassion for the child or teen, our brains may be more reactive to parents. Watch for the above signs in yourself too. Instead of letting shame and defensiveness take over, reach out for help from a supervisor, mentor, or trusted colleague.
As with so many things, an ounce of prevention is worth a pound of cure. Some of the same strategies that help children overcome blocked trust can prevent and treat blocked care.
- Increase playfulness. Little games that involve safe touch or joyful eye contact boost the feel-good hormones in both parent and child.
- Find or create a community that “gets it” without getting stuck. Many parents feel alone with their shame until they are able to hear that what they are dealing with is normal and others have walked the path before them.
- Nurture curiosity and compassion. When uncomfortable feelings come up, notice them. Chances are, they have helped you survive. Thank that anger or fear for its work in your life and let it know that you are okay without it for the moment.
- If you are involved in training parents, be sure that blocked care and blocked trust are topics you are spending time on, both in preparation for placement as well as in ongoing support.
Reframe the Narrative
All too often, discussions during therapy sessions and home visits revolve around behavior, specifically undesirable behavior. The story that starts to emerge is, “This is a bad kid who does bad things.” Add to that the feeling of failure so many parents experience, and the story hiding in the shadows is, “…and I’m a failure because I can’t help them heal.”
With what we know about trauma and the brain, let’s reframe the narrative.
- Instead of a scary story about a bad kid, it is a sad story about a brave, loveable, vulnerable kid.
- When the teen says, “I don’t need anyone,” we might respond by saying, “You were so smart and resourceful to figure out how to survive on your own. It probably feels really uncomfortable to get close.” With a little smile and compassion add in, “…even though we all need closeness.”
- Parents are often telling themselves, “I’m a failure.” Let’s help them hold a different story: “I’m doing my best at a hard job, and it’s normal to need help. I am part of helping my child heal and grow.”
- As professionals in the field, let’s remind ourselves that these are brave kids and strong parents working together with to get through some really tough stuff.
Take a few deep breaths before you interact with a child (or parent) and remind yourself of the real story. Perhaps write it on a sticky note and put it on your computer screen. Tell a trusted friend or colleague how you are reframing the narrative so you can reach out for a reminder when your brain is stressed and tired.
Tending to Your Brain and Body
This work requires us to have a well-regulated nervous system. You cannot give what you do not have. As much as it feels like a luxury sometimes, true self-care—nurturing your mind, body, and soul—is a necessity! We know that parents must tend to their brains and bodies if they are going to be able to help their child heal. The same is true for professionals.
While crises, staff and resource shortages, and the emotional intensity of this work certainly present obstacles, we must continue to find moments to breathe, take a break, nurture our bodies, and heal our souls. If not, we won’t have the upstairs brain power to implement any of these practical strategies for preparing and supporting children.
Want to bring more brain-based support to your agency?
I founded BraveBrains to equip adults and empower kids on the path to healing. Reach out to info@BraveBrains.com for more information on how we can be a support! Bulk discounts are available on posters, bears, and therapeutic card games. Not-for-profit agencies may qualify for as much as 50% off Riley the Brave books!
We also offer professional development, parents’ nights, family events, and more! Click here to learn more or find an upcoming event near you!